Beginnings
Prior to the 1960s, failing kidney function was a guarantee of death. Kidney failure was a fatal condition as neither long-term dialysis nor kidney transplantation were feasible treatment options.
Healthy kidneys remove waste and excess water from the blood, but if the kidneys fail, dialysis is needed to remove the excess waste. Dialysis at that time was used only to stabilize a patient. If the kidneys did not begin to function correctly the patient would eventually die of kidney failure.
Patients could not undergo dialysis treatment indefinitely due to the glass shunts used in the treatment. The shunts caused damage to veins and arteries to such a degree that long-term dialysis was impossible.
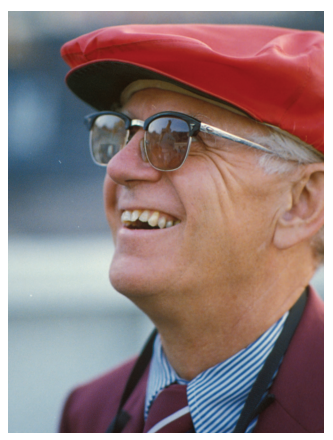
The Division of Nephrology was established in 1958 with the recruitment of Dr. Belding H. Scribner from the Mayo Clinic to the University of Washington.
The 1960s
Dr. Scribner and his team at the University of Washington modified glass dialysis shunts by making them from Teflon.
The Teflon Scribner Shunt worked by keeping the circulatory access open after dialysis treatment. The kidney dialysis machine could be attached to the tube whenever necessary without damaging the veins or arteries.

1962
With the creation of the Scribner Shunt, ongoing dialysis treatment became a reality, and patients with chronic kidney disease could live with the disease.
Scribner then worked with the King County Medical Society to establish the Seattle Artificial Kidney Center with Dr. James Haviland, and in January 1962 the first outpatient dialysis facility in the world was opened. Later it was renamed Northwest Kidney Centers.
However, hemodialysis remained a scarce resource through the 1960s, and treatment was available only to people selected for dialysis by the “Life or Death Committee”, which laid the foundation for modern bioethics.

1969
Linda Johnston was a young patient from Bellevue, WA, in need of dialysis in 1969. Her case came before the “Life or Death Committee.”
Read Linda's inspirational story:

The 1970s
1970
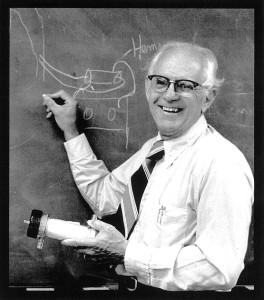
Research by Dr. Henry Tenckhoff and Dr. Fred Boen resulted in peritoneal dialysis being offered by the Northwest Kidney Centers. Dr. Tenckoff introduced an indwelling peritoneal dialysis catheter that remains the most widely used catheter to date and bears his name.
1973
To maximize the access to lifesaving therapies, Scribner also worked tirelessly with colleagues nationwide to persuade the US Congress to enact the only disease-specific coverage by Medicare in 1973 that has forever changed the clinical practice of nephrology.
1979
Dr. Robert O. Hickman created the Hickman catheter (double-lumen silicone rubber Dacron cuffed catheter), for ambulatory home PN and chemotherapy.
Oral History
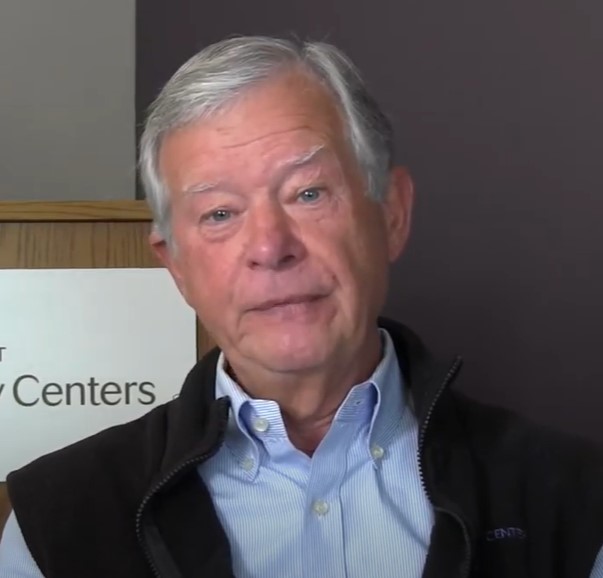
In the early 1970s, Dr. Mike Kelly moved to Seattle to work at the UW Medical Center.
In this video interview, Dr. Kelly remembers his early career working with Dr. Belding Scribner and the team of dialysis pioneers in the Division of Nephrology.
The 1980s
1989
Northwest Kidney Centers was the first site for human studies on erythropoietin.
View the Special 40th Anniversary Grand Rounds session in honor of Erythropoietin Clinical Trials in Seattle, featuring talks by Drs. Ian de Boer, Michael Kelly, Matt Rivara, John Stivelman, and Kleber Fertrin.
The 2000s
2001
First altruistic (non-directed) living kidney donation at UW Medicine
Learn about Linda Herbert and her decision to donate a kidney to a stranger
2008
Kidney Research Institute is established as a leading clinical research endeavor focusing on the early detection, prevention, and treatment of kidney disease and its complications.

2011
The Center for Dialysis Innovation begins with a vision to revolutionize kidney dialysis.

Legacy
For his work, Dr. Scribner received the Gairdner Foundation International Award in 1969 and the Albert Lasker Award in 2002 for major contributions to medical science.
The impact of the work done within the division is further underscored by the American Society of Nephrology conferring the Belding H. Scribner Award, named after our first division head, to one or more individuals who have made outstanding contributions that have a direct impact on the care of patients with kidney diseases or have substantially changed the clinical practice of nephrology.
Ongoing research
Our work continues today with translational and basic research, clinical trials, improvements in technology, and the desire to improve the lives of kidney patients.



