AKI consults
While on your nephrology rotation, you will see many consults for acute kidney injury (AKI). In many cases, the reason for AKI is quite clear, although you will also see plenty of AKI cases with more occult causes that require in-depth investigation. It is important to go through a thorough differential in order to diagnose and manage these cases. This goes beyond the pre/intra/post-renal paradigm.
Remember, one of the most important questions to ask when receiving an AKI consult is “Is the patient urinating?”
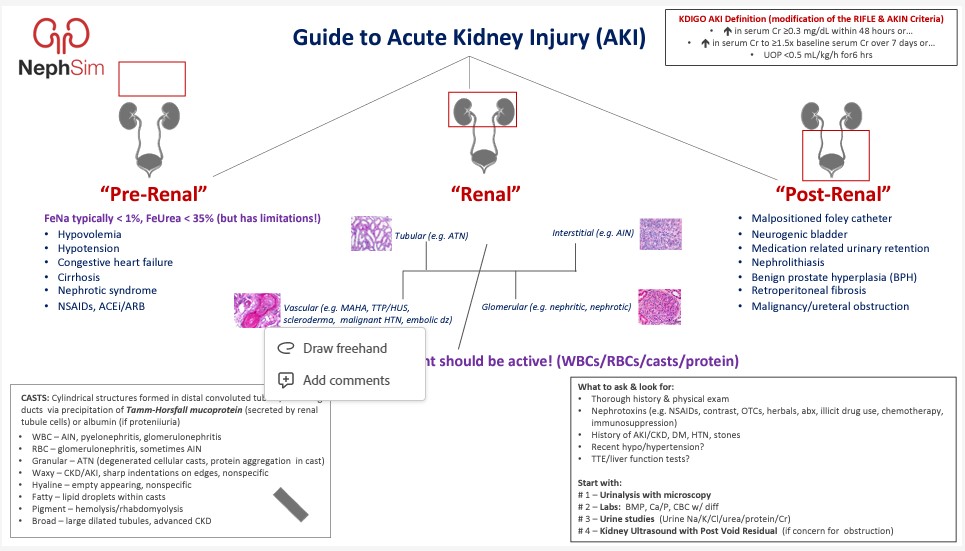
Guide to Acute Kidney Injury (AKI)
To start, we recommend reviewing the following slide from NephSim which gives a nice overview of the various categories of AKI, and the specific diagnoses to consider within each category.
Nephrology for the Non-Nephrologist: Acute Kidney Injury
with Dr. Benjamin Broome, Dr. Elizabeth Edwards, and Dr. Donald DiPette
Next, listen to this podcast which provides a brief overview of AKI.
Management of Acute Kidney Injury: Core Curriculum
by Peter K. Moore, Raymond K. Hsu, and Kathleen D. Liu
This Core Curriculum from AJKD goes through the various causes and management of AKI in more detail. You do not need to commit this to memory, but it should help serve as a guide when thinking through these cases.
Now that you have gone through some background information, you can work through a couple of AKI cases that you may see while on service.
If you are on a Harborview Medical Center rotation, you will likely see a case like this:
NephSim - Case 4
A 33-year-old man with no known medical problems presents to urgent care complaining of diffuse muscle pain (myalgias) and fatigue. He went to an indoor cycling class a few days ago and though his muscles were sore from the class, but the pain has gotten worse since then despite taking NSAIDs “around the clock.”
If you are on a UW Medicine Montlake rotation, you will likely see a case like this:
NephSim - Case 38
A 47-year-old woman with a history of hypertension and a recent diagnosis of acute myeloid leukemia (AML) presents with fatigue, fevers, nausea, vomiting, and diffuse body aches.